Herniated disc

Lumbago, herniated disc and percutaneous or endoscopic discectomy
Back pain (low back pain) is a very common symptom and is the most common cause of absence from work in adults. 75% of adults will experience back pain at some point in their lives with 3% experiencing pain that extends down the leg. In a proportion of these patients the pain is due to a herniated intervertebral disc (or herniated disc). An intervertebral disc herniation is caused when a small part of the intervertebral disc (material that is sandwiched between two vertebrae) presses on the adjacent nerve, resulting in leg pain (sciatica) or pain in the lumbar region. The most common treatment intervention is conservative (involves bed rest for a few days and painkillers).
Indications for surgery are:
- failure of conservative treatment (painkillers and restriction of activities)
- the existence of severe drug-resistant pain (the patient can no longer tolerate it)
- weakness in the leg
- cauda equina (hypersensitivity or pain in the genital area accompanied by weakness in the legs or inability to urinate or defecate)
- The patient's need to return to daily activities or work without pain as soon as possible.
Surgical intervention
If conservative treatment fails, various surgical interventions are available which usually provide immediate relief. Surgical intervention nowadays is performed with the most modern technology (minimally invasive surgery).
The newest minimally invasive technique in the spine (for lumbar and cervical herniated discs) is percutaneous microdiscectomy. This procedure can be combined with the latest neuronavigation techniques that allow the neurosurgeon to locate the intervertebral disc and to be accurate to the nearest millimetre in each operation.
Even less invasive is the percutaneous endoscopic transforaminal discectomy, where, using an endoscope and a very small skin incision of 5-6 mm, the part of the disc that protrudes and presses on the nerve root is removed.
Advantages
- Procedure under local or general anaesthesia.
- Mobilisation 3 hours after surgery.
- Discharge from hospital a few hours after surgery.
- Reduced back or neck pain (because there is no tissue injury during surgery).
- Return to daily activities in a few days.
Unlike traditional discectomy techniques (lasting 1 hour) that require an incision in the spine - dissection of the muscles - and major injury to adjacent tissues, minimally invasive techniques (percutaneous and endoscopic discectomy) are characterized by zero injury to the muscles (they are dissected with microtubes instead of being cut) resulting in the ability to mobilize and discharge from the hospital the same day.
These procedures are the most popular in major hospitals in America and Europe, where the traditional open method has been abandoned.
The effectiveness of minimally invasive techniques reaches 98% in organized centers and is routinely applied in our clinic with more than 500 similar procedures since 2013.
Specific indications
- Patients who wish to quickly return to daily activities.
- Athletes with a requirement for a quick return to sporting activity.

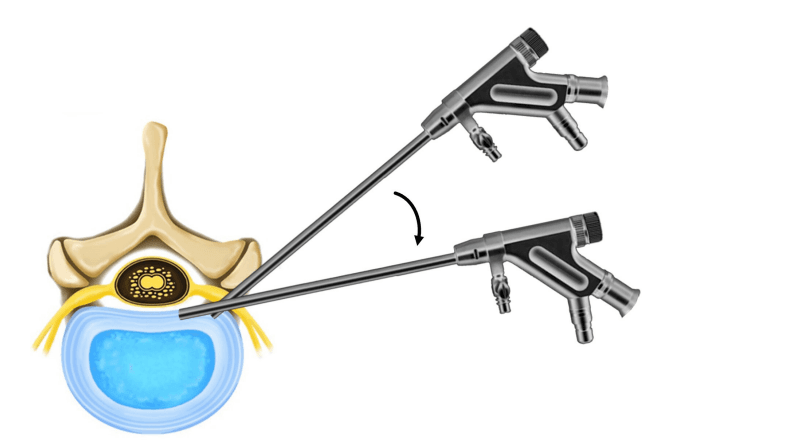
Endoscopic percutaneous perforated discectomy.
Preoperative disc herniation MRI in a patient with back and leg pain.

5 mm skin incision in endoscopic percutaneous perforator discectomy.

Intraoperative imaging of percutaneous microdiscectomy.
Schematic image of endoscopic discectomy.
Postoperative image of 1 cm skin incision.
