Cervical myelopathy

In cervical myelopathy we have damage to the spinal cord at the level of the cervical spine. The most common cause is pressure from a cervical herniated disc or osteophyte (cervical spondylosis). Other causes may be the presence of a tumour, demyelinating lesion, haematoma, traumatic injury, etc. The patient presents with weakness or numbness in the arms or legs with accompanying spasticity, increased reflexes and difficulty in walking.The diagnosis is clinical (by the neurologist or neurosurgeon) and is based on the characteristic clinical picture and confirmed by cervical MRI. The disease is progressive and leads to disability.
The operation may be anterior (anterior cervical microdiscectomy) or posterior (pediclectomy with or without spinal fusion) and depends on the type of anatomical lesion, the biomechanical analysis of the case and other factors.
At the University Hospital of Rio Patras we have the highest technology required for spinal diseases such as O ARM intraoperative CT scan, Stealth Station neuroplanning and new generation Leica microscope.
The role of the neurosurgeon is early diagnosis and treatment of the condition. Treatment is surgical and involves removal of the herniated disc (or osteophyte) with microdiscectomy and possibly spinal fusion. Success in treatment lies in stopping the deterioration of the myelopathy.
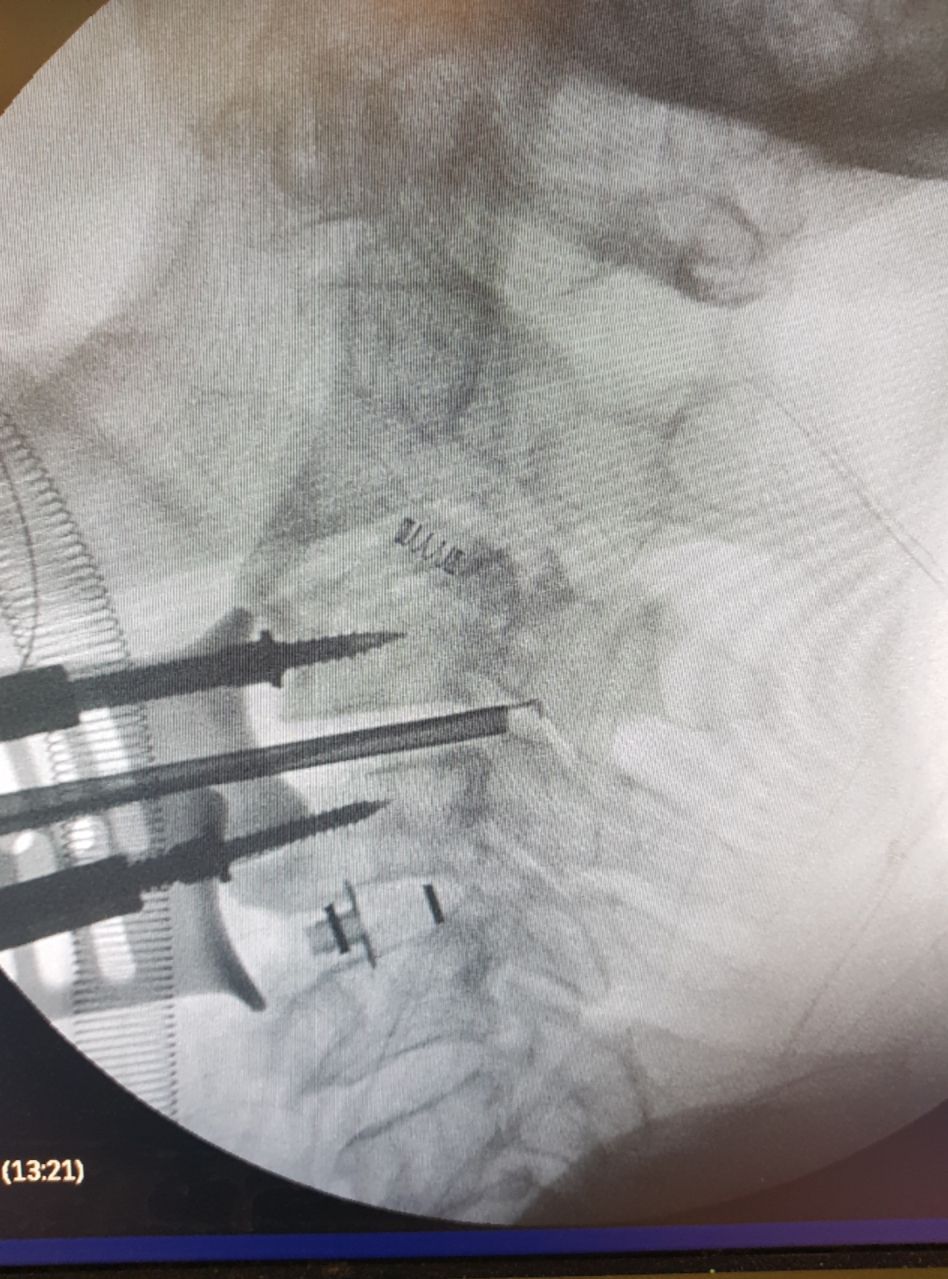
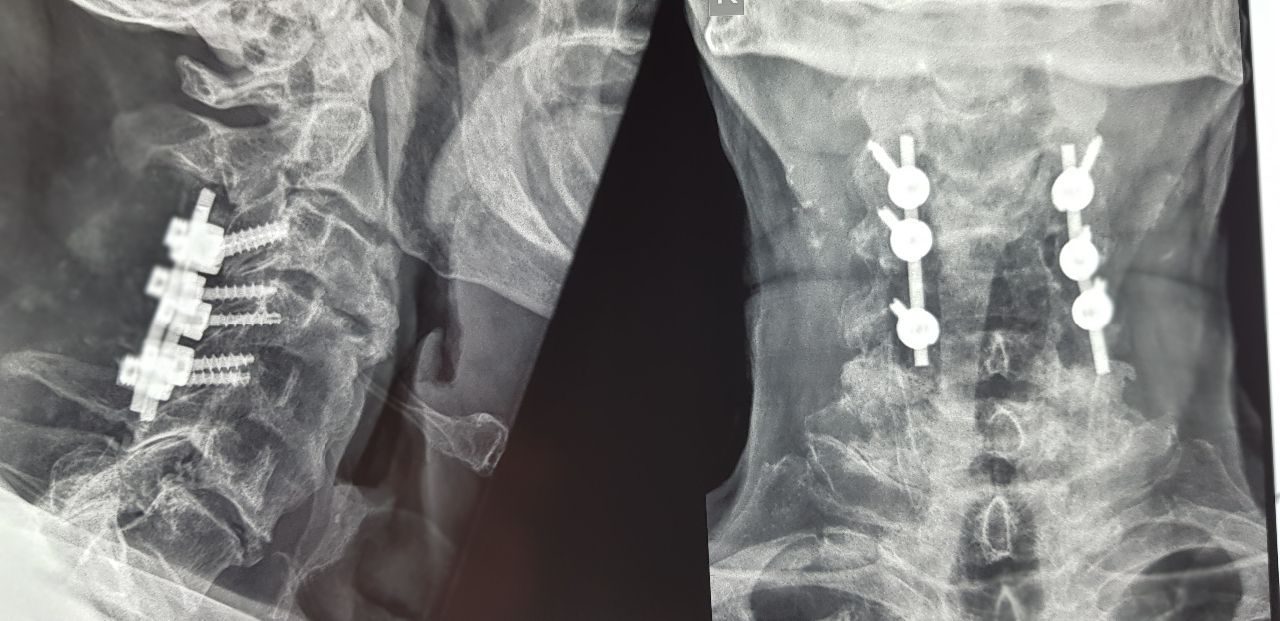 Posterior cervical spinal fusion of lateral lumps and pediclectomy in extensive myelopathy.
Posterior cervical spinal fusion of lateral lumps and pediclectomy in extensive myelopathy.
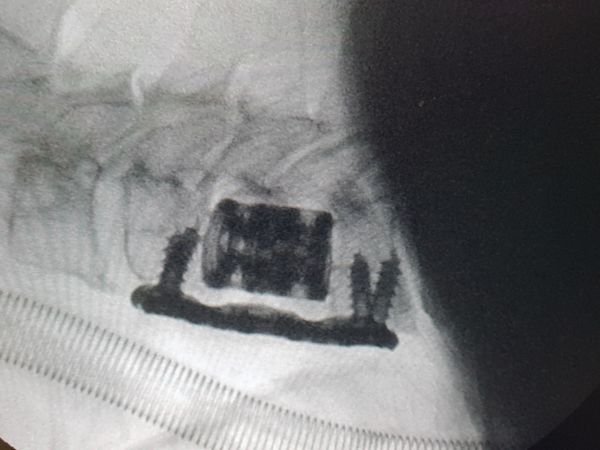
 Anterior cervical microdiscectomy in two planes with cage placement.
Anterior cervical microdiscectomy in two planes with cage placement.
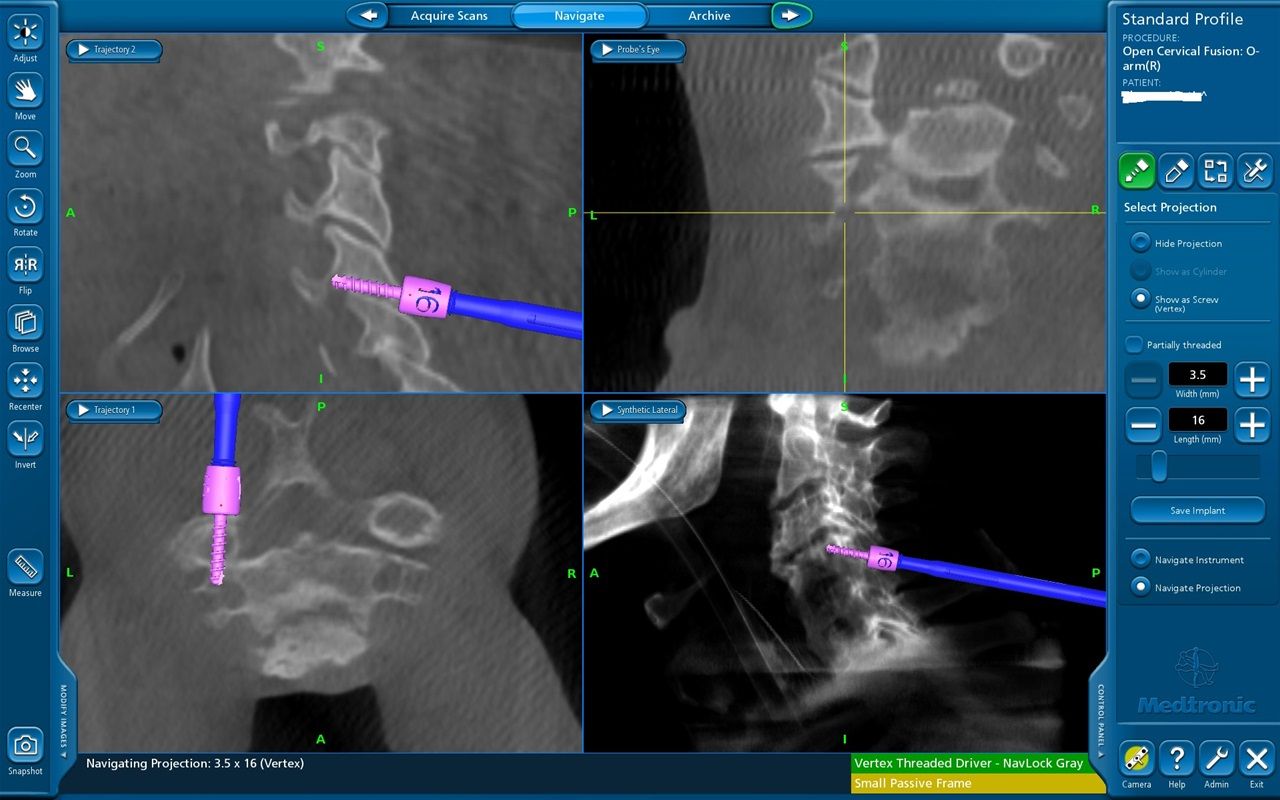
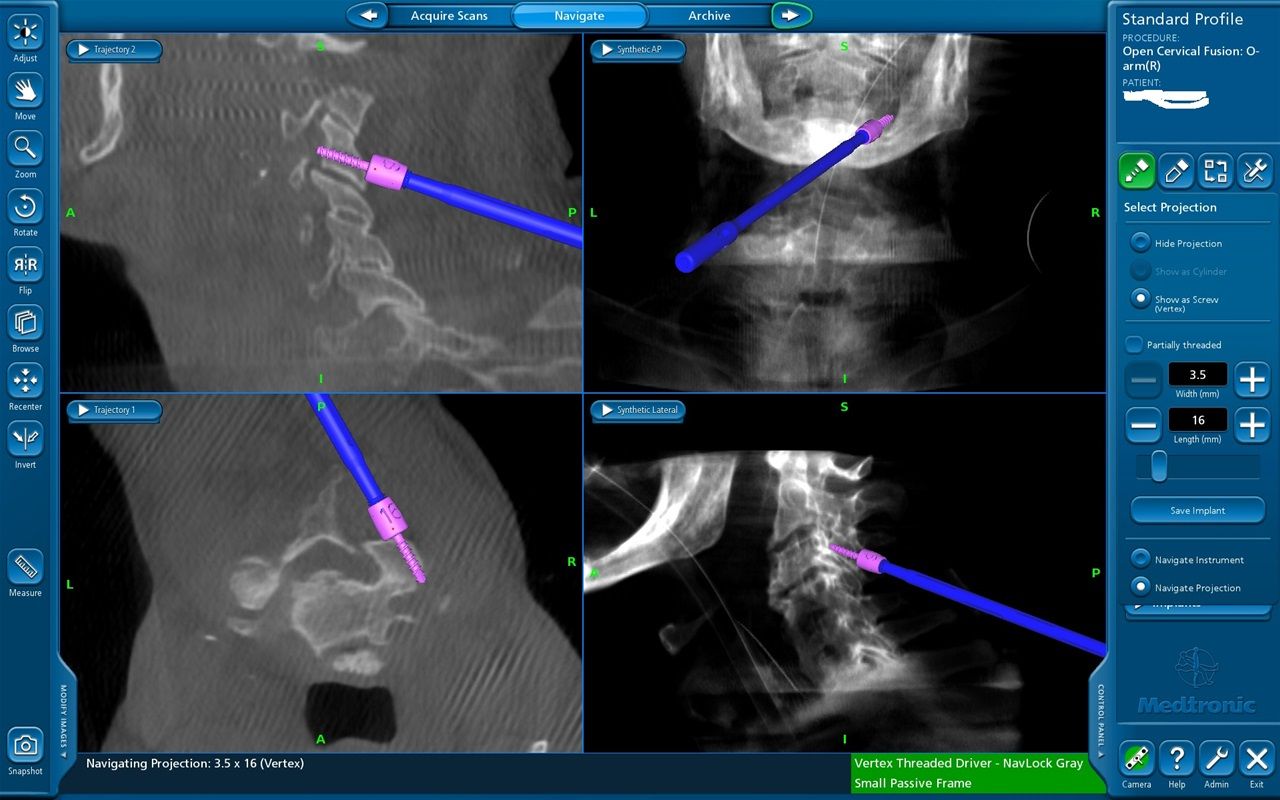
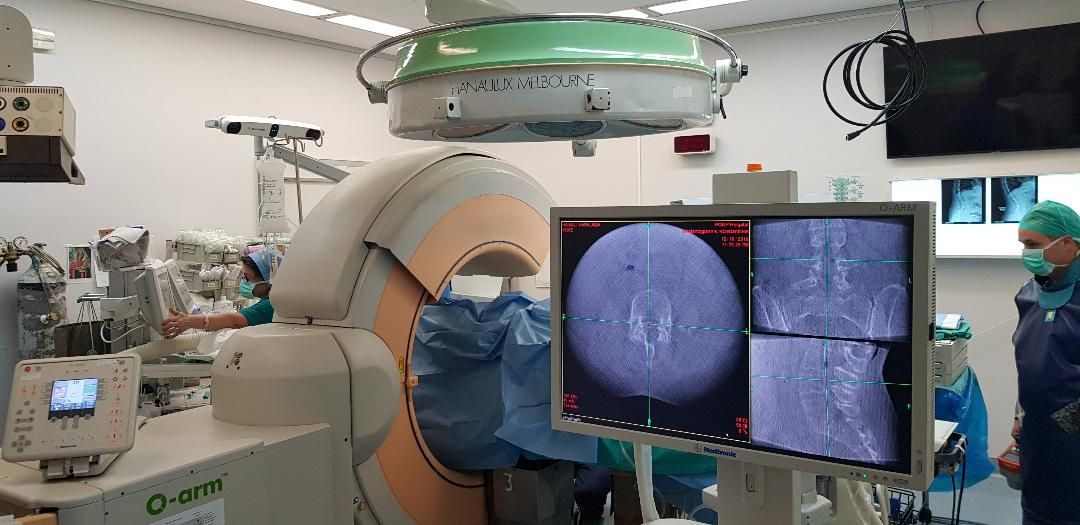 Neuroplanning with Stealth Station and intraoperative imaging with 0 ARM.
Neuroplanning with Stealth Station and intraoperative imaging with 0 ARM.
 Interventional cervical discectomy and spinal fusion in severe myelopathy.
Interventional cervical discectomy and spinal fusion in severe myelopathy.
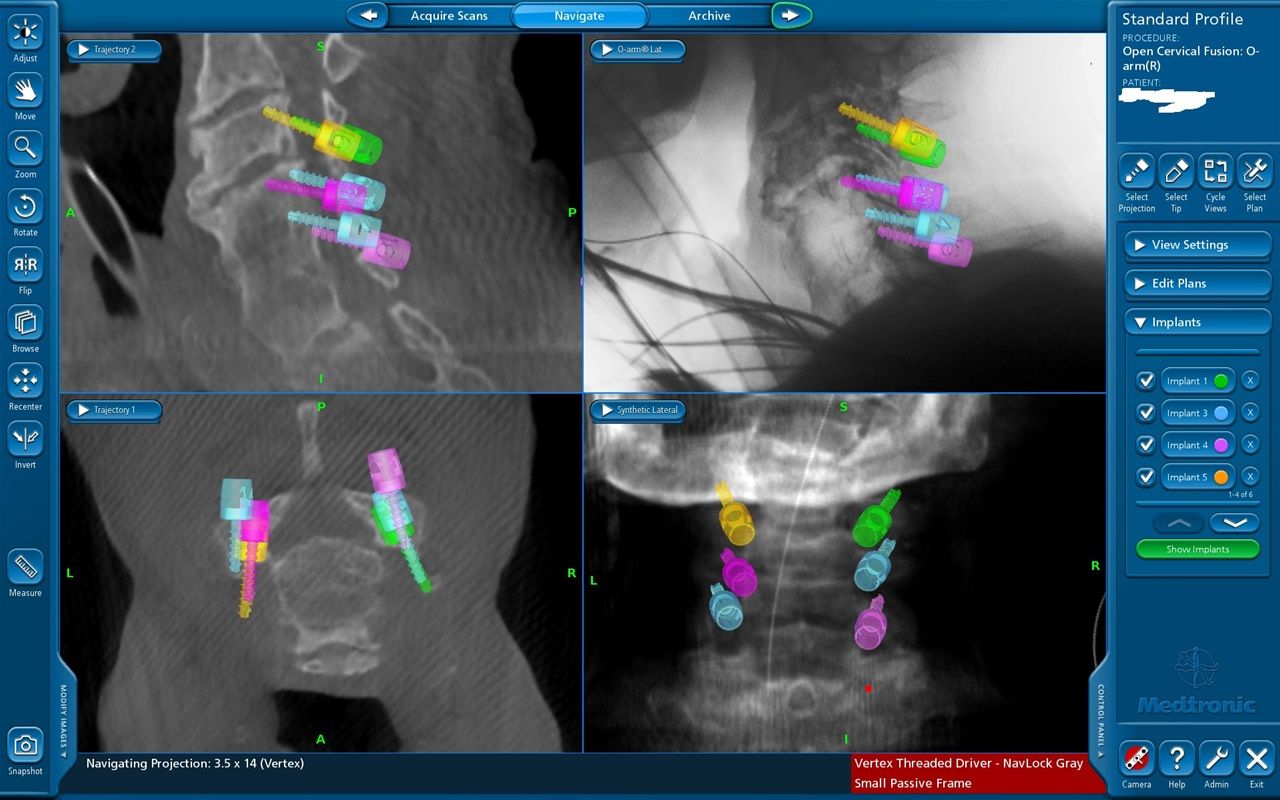
 Intraoperative imaging of posterior spinal fusion of the ACL with O ARM
Intraoperative imaging of posterior spinal fusion of the ACL with O ARM
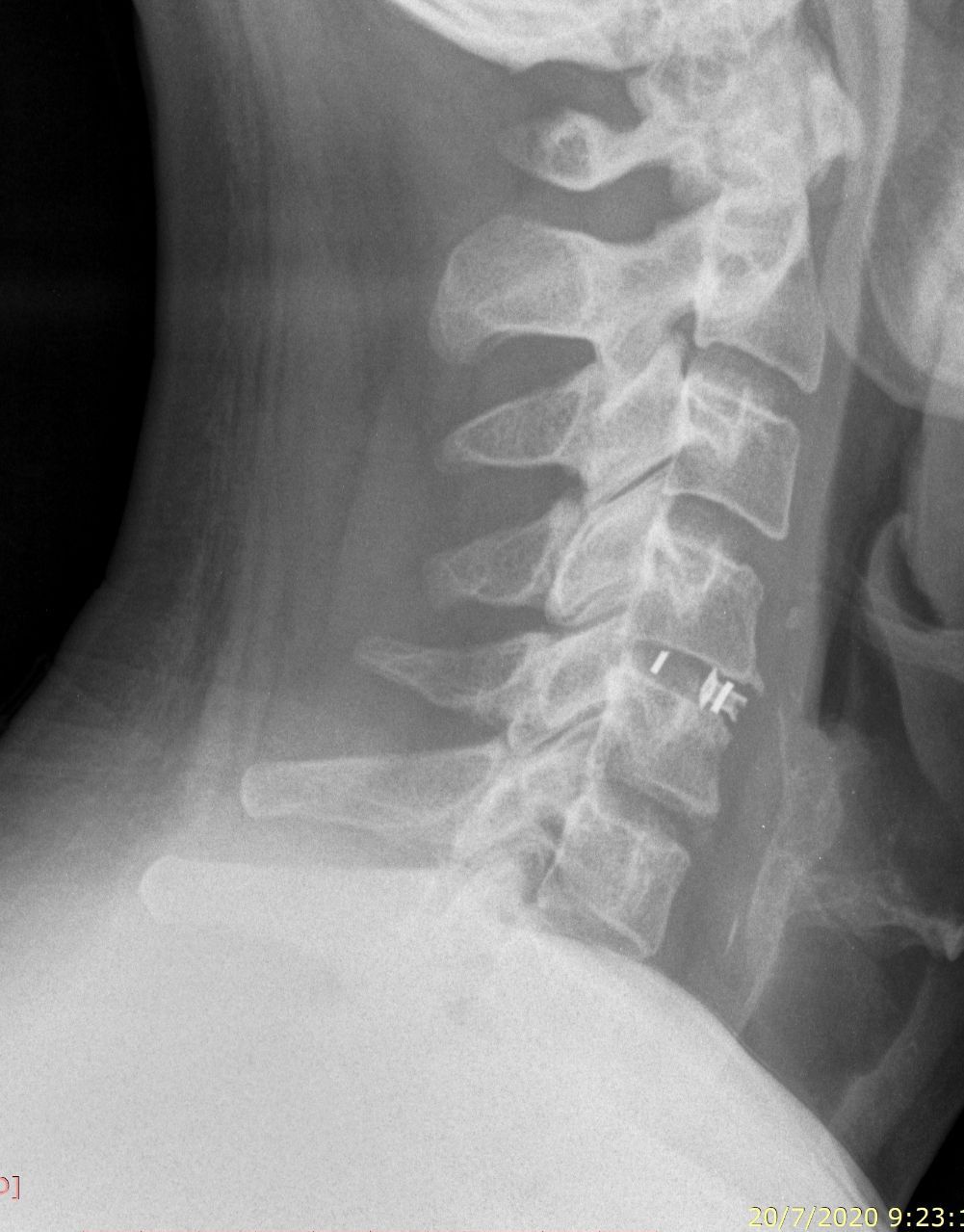 Cervical microdiscectomy and spinal fusion A5-6 with cage.
Cervical microdiscectomy and spinal fusion A5-6 with cage.
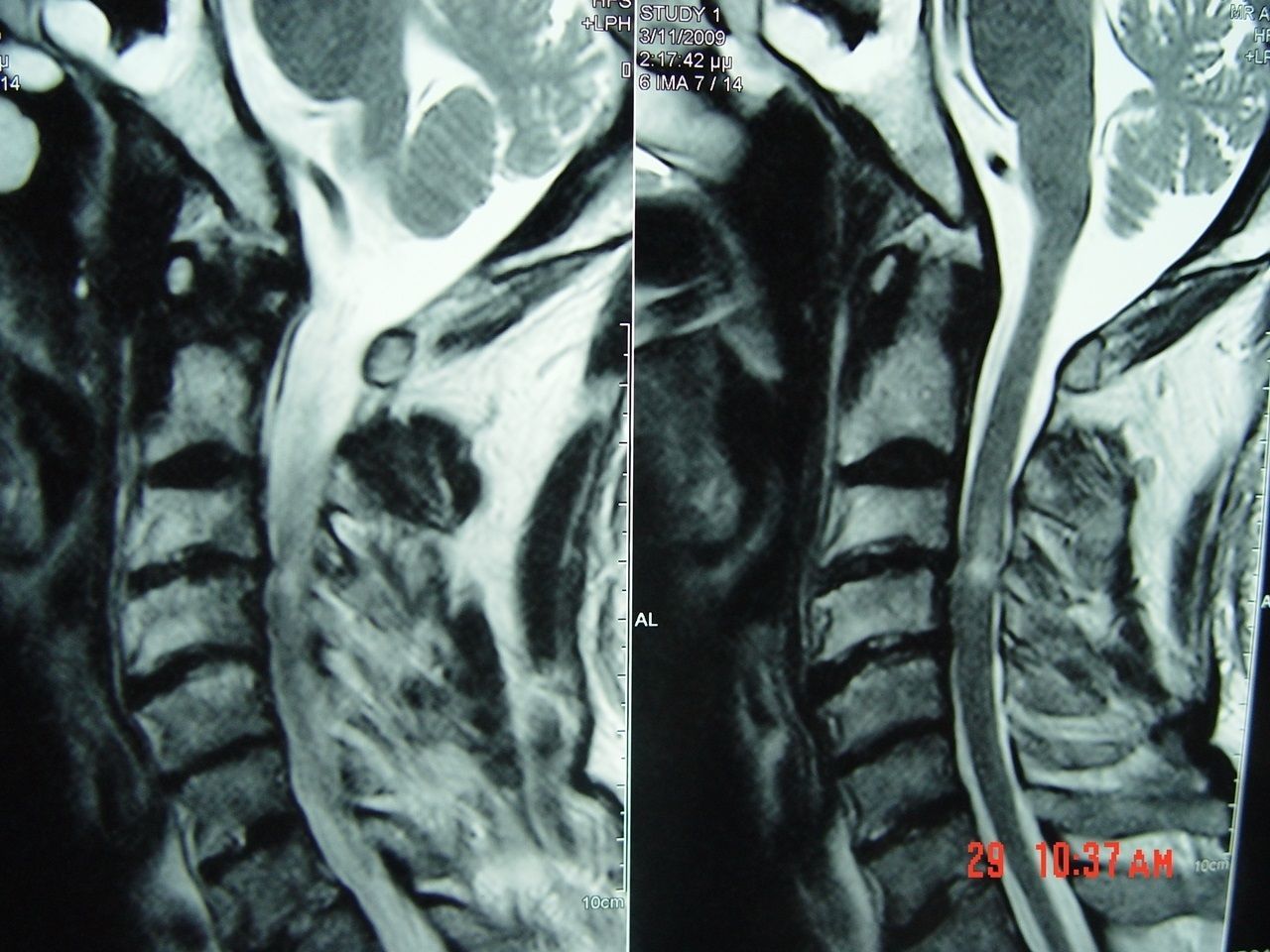 Cervical myelopathy A3-4 with the characteristic signal on MRI.
Cervical myelopathy A3-4 with the characteristic signal on MRI.