Parkinson's disease

About 4,000,000 people in the world suffer from idiopathic Parkinson's disease. In the USA there are an estimated 1,000,000 Parkinson's patients and 60,000 new cases are reported each year. Because the average life expectancy is increasing, it is estimated that the incidence of the disease will increase fourfold by 2040. The average age of onset is 60 years.
The cause of the disease is thought to be the progressive degeneration of dopaminergic neurons in the medulla oblongata, which produces the dopamine necessary to regulate the functioning of the basal ganglia. A 60-70% degeneration of these neurons is required for the disease to occur.
Deep brain stimulation (DBS)
The breakthrough in the results of surgery for DBS. The breakthrough in the results of Parkinson's surgery came in the 1990s, with the introduction of MRI and improved pacemaker technology. Deep brain stimulation with high frequency electrical stimulation is now a rapidly developing surgical technique for the symptomatic treatment of motor disorders (Parkinson's disease, dystonia, idiopathic tremor). The electrical stimulus has a specific frequency (90-180 Hz), intensity (0.1-10 volts) and range (60-450 msec). This technology is based on the insertion, under local anaesthesia, of an electrode into a nucleus of the brain (thalamus, or macula, or hypothalamic nucleus) and the continuous stimulation with a current from a battery placed in the anterior chest wall. The electrode has 4 poles, each of which acts as an anode or cathode allowing the electrical stimulus to be transmitted or received.
Changing the polarity of the electrode (done by the therapist with a laptop computer) causes a change in the patient's symptoms. The implantation of the electrode is based on coordinates on the MRI, use of computer neuro navigation (Stealth station-FrameLink software) and intraoperative recording with microelectrodes (Lead Point) . The mechanism of action of deep brain stimulation remains unknown. There are several theories based on studies in experimental animals and intraoperative stimulation in humans. An oversimplified theory claims that the action of the method is exerted through neuronal suppression resulting in the re-regulation of dysregulated neuronal circuits in the brain.
An estimated 40 000 patients worldwide have undergone this procedure. Most of them enjoy a better quality of life.
Brain targets for DBS
The results of DBS depend on the site of electrode implantation. There are three common target sites for controlling movement disorders: the thalamus, the macula and the subthalamic nucleus. Each target has different indications, effects and possible complications.
The thalamus (Vim)
The anterior medial nucleus of the thalamus is the target of choice for reducing tremor regardless of its etiology. The most common indications are Idiopathic Tremor and Parkinsonian Tremor, but tremors from other causes such as MS, strokes and trauma have been treated at our hospital. Benabid was the first to treat Parkinsonian patients with drug-resistant tremor by applying DBS in the ward. This procedure was widely accepted and received FDA approval for DBS technology on August 4, 1997. Studies have shown that DBS is as effective as thalamotomy and has fewer potential complications.
A recent multicenter study showed that DBS in the chamber can reduce tremor by 85% at one-year follow-up. Upper and lower limb tremor can be reduced with improvement in the score of activities of daily living. In our clinic we apply DBS in the ward and many patients enjoy benefits from the procedure at a rate of over 95%.
The Macula (Gpi)
The macula is the target of choice for the symptoms of Parkinsonian dyskinesia. Recently it has also been used for dystonia of various causes. Macrodotomy (permanent damage to the macula) became very popular again for the treatment of Parkinson's disease after 1992. This operation dramatically improves unilateral dyskinesia and, to a lesser extent, bradykinesia, tremor and pain. However, as the disease progresses, the other side of the body is often affected. Most, but not all, neurosurgeons were reluctant to perform unilateral ototomy because of the high mortality rate observed after bilateral thalamotomies.
DBS of the macula offered a solution. As in the case of ototomy, the most spectacular effect of macular DBS is the reduction of unilateral dyskinesia. Reports of the beneficial effects of DBS in dystonia offer hope for this debilitating disease. In our clinic we are applying the above technique to patients with dystonia with encouraging results.
The Subthalamic Nucleus (STN)
The hypothalamic nucleus is the target of choice for all symptoms of n. Parkinson's disease. Its hyperfunction is considered a critical abnormality of the Parkinsonian brain. The reversible effects of DBS, made STN DBS more appealing than causing permanent damage. Unilateral stimulation of the hypothalamic nucleus mainly affects the unilateral hemisphere. Benabid reports improvement of all major Parkinson's symptoms: bradykinesia, stiffness and tremor, after bilateral DBS. Patients also experienced reduced motor fluctuations and reduced need for medication. A double-blind study conducted by Kumar and colleagues yielded similar results. They reported a 65% reduction in off , 40% improvement in on , and 85% reduction in levodopa-induced dyskinesias. In our clinic there is extensive experience in applying DBS to the subthalamic nucleus with an improvement in Parkinson's disease symptoms of over 75%.
Complications
Complications with the use of DBS are minimal and usually reversible. Implantation of a foreign object under the scalp of an elderly patient with marginal nutrition can cause infection. Symptomatic bleeding at the target site of the electrode is a small possibility. The benefits of the procedure and potential complications are discussed in detail before the decision to operate is made.
Conclusions
At the University Hospital of Rio Patras there has always been close collaboration between neurologists and neurosurgeons dealing with Parkinsonian patients. Patients with drug-resistant symptoms have the possibility to benefit from a variety of surgical interventions. In the future, there may be new treatments such as nerve cell transplantation, gene therapy and growth factor injection. Each new treatment will bring clinical benefits to our patients and a greater understanding of Parkinson's disease.
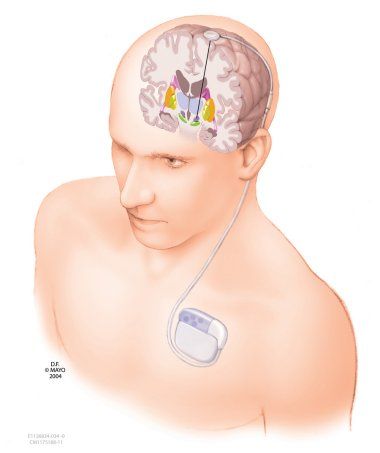 Figure 1.* Illustration of the DBS device. The device resembles a pacemaker and is placed in the chest, the electrode is placed on the preselected target in the brain.*
Figure 1.* Illustration of the DBS device. The device resembles a pacemaker and is placed in the chest, the electrode is placed on the preselected target in the brain.*